Investigating violence prevention and healthcare workplace violence programs

Employees in healthcare are 20 times more likely to experience workplace violence (WPV) than any other profession, and that statistic continues to rise in the United States. Here, we will explore if the violence prevention climate (VPC) affects a healthcare workplace violence program, as well as introduce five studies comparing two questions followed by suggestions for alternative studies to further this research:
- Are there differences in perspectives between healthcare employees and managers regarding the WPV program?
- If so, how do employee perspectives affect the WPV program?
Due to the rising epidemic of healthcare workplace violence, the National Institute for Occupational Safety and Health (NIOSH) published WPV prevention guidelines to enhance hospital programs in an attempt to decrease risk and injury. The WPV guidelines consist of several elements: management and employee commitment through a zero-tolerance policy, workforce violence prevention training, post-incident investigation documentation, staffing and evaluation. While there is a significant amount of research conducted on WPV, this article selected studies in the U.S. from within the past two decades that focus on whether healthcare employee perspectives impact the safety climate.
Research
Study 1: Management Actions Impact Violence Climate
The research article by Paul Spector et al. titled "Perceived violence climate: A new construct and its relationship to workplace physical violence and verbal aggression, and their potential consequences" is a cross-sectional quantitative study conducted at one hospital and investigated whether management's actions impacted the perceived violence climate. The Spector et al. study assessed two hypotheses:
- High perceived violence climate results in lower experiences with violence, injury and perceived danger.
- Experience with WPV would impact physical and psychological strain.
There were no documented exclusions to the participants or surveys. The study limitations consisted of being a one-time cross-sectional and self-reported study with potential response bias and a newly developed tool.
The study developed a 7-item scale by Spector et al. to measure the perceived violence culture, later known as the VPC scale. Along with the VPC questions, the study asked additional 20 questions on work safety, physical and psychological strain. The Spector et al. study consisted of 98 nurses who were all women, mostly registered nurses (53%), 30 years of age or older (88%) and had more than 10 years of experience (64%) working at one Florida hospital.
The study supported both hypotheses and found a positive violence climate is one where management has adopted workplace violence policies and procedures, workforce violence prevention training and useful interactions between coworkers and management. The results suggest management directly affects the facility's workplace violence program and safety culture. Further studies should explore the impact management role plays in the safety climate.
Study 2: Relationship between Climate and Employee Satisfaction
The research article, “Organizational violence and aggression: Development of the three-factor Violence Climate Survey,” by Stacey Kessler et al., is a cross-sectional study examining the relationship between the violence climate and participant experiences with workplace violence. The study assessed six hypotheses relating to the VPC, psychological strain and workload. Kessler et al. recruited participants through a centralized online survey database. There were no documented exclusions to the participants or surveys. Limitations consisted of being a one-time cross-sectional study assessed individual perceptions rather than a shared climate perception. Participants may have a self-selection bias based on their community or past experiences.
The study consisted of 49 questions with several demographic questions followed by violence safety climate (VSC), management safety climate (MSC), psychological, physical and workload questions. Participants were psychology university students working in various industries such as healthcare, sales and hospitality. The study had 216 participants: 81% were women with an average age of 24 years old (range from 18 to 57).
The results of the survey supported the hypotheses negatively correlating VPC to both psychological strain and workload. The study results suggest a lower VPC and higher stressors impact patient care quality and employee satisfaction. Researchers should consider further investigation around the impact of physiological stresses and VPC's impact on the culture.
Study 3: Relationship between Perception of Violence and Risk
James Blando et al. conducted a cross-sectional study of emergency department and behavioral health nurses to assess their perception of violence based upon their safety climate and whether this correlates with the risk of injury or harm. The study, “Impact of hospital security programmes and workplace aggression on nurse perceptions of safety,” included topics on the violence training program, policies, management support and reporting.
The hospitals selected, located in California and New Jersey, represent a sample of most hospital demographics in U.S. 300-bed trauma and general acute care hospitals and less than 300-bed general acute care facilities. The participants include 168 emergency department and 73 behavioral health unit nurses. The study design consisted of 15-minute interviews and a review of employee injury reports. The limitations included the timeframe of assault reports and staff interviews, which were three years apart, which could affect some of the results.
The study asked seven questions: two were demographic questions, and five focused on perceptions of safety. The safety questions include, "Received violence-based safety training," "Felt security guards are adequately trained and experienced," "Felt security and staff worked together during events," and "Felt security was of high importance to management." Over 80% of participants had more than five years in the healthcare field and greater than one year in their current role.
The results of the study reported that 86%t of the emergency department and 100% of behavioral health participants received violence training. In addition, 27% of emergency department participants and 59% of behavioral health participants received regular violence training updates. Blando et al. found all participants experienced WPV; yet, behavioral health participants had more training, felt safer, and had lower violence incidents. The study determined some of the participant's safety elements (e.g., security or law enforcement presence) did not reduce actual risk or injury, only the injury's potential severity. Lastly, Blando et al. suggest further investigation into management's impact on quality and employee turnover and identify which elements can reduce the risk of violence as perceptions between employees and managers differ.
Study 4: WPV Impact on Employee Perceptions
The research article “Perceptions of managerial support after workplace violence” by Wanda Christie is a phenomenological qualitative study of nurses working at a hospital to learn more about their emotions and perceptions of the violence prevention climate. Christie excluded participants from the study if they were under 18 years of age, under medical care for injuries due to violence or were diagnosed or receiving treatment for a psychiatric disorder due to the event. Due to the limited sample size of the participants, there is a high likelihood of selection and detection bias all from one hospital department.
The study consisted of interviewing thirteen emergency room registered nurses from a 434-bed level-one trauma teaching hospital. The interviews ranged from 45 minutes up to two hours in length. The interview began by asking the participant to describe an event, what occurred after the event and how they currently feel about violence and the safety culture.
The results of Christie's study found three major themes aligned with OSHA's WPV elements: leadership, policy and training. OSHA's WPV program recommends manager support and accountability to foster a safety culture by developing a zero-tolerance policy. Christie's study participants reported:
(a) Their managers did not care about their well-being due to a lack of follow-up on their personal safety and lack of actions (post-incident investigation and removal of the patient) after violent events. In addition, managers did not discharge or kick out violent patients; however, they did conduct post-event investigations; unfortunately, they were not long enough.
(b) They have a zero-tolerance policy; however, managers were not in compliance and not held accountable, as they did not kick outpatients that assaulted the nurses.
(c) "All [nurses] said that the CPI training was ineffective" for them and more effective for security because security manages the violent events (p.34). While leadership, policy and training aligned with OSHA's WPV guidelines, the implementation was not as effective as the safety climate is not supportive of the program.
Study 5: Relationship between MSC and VPC
The research article by Linda Hamblin, titled “Management safety climate and violence prevention climate: A mediational model for healthcare employee outcome,” is a cross-sectional quantitative study consisting of two sample populations investigating the relatedness and differentiation between the management safety climate (MSC) and the VPC and whether the MSC impacted the VPC. Hamblin suggests that VPC is the perception the facility promotes to prevent violence. The study assessed seven hypotheses relating the different climate studies to each other. Sample one consisted of 224 healthcare professionals. The second sample consisted of 446 hospital employees who work predominately in the intensive care unit, surgery, psychology, emergency department or security in the hospital system with over 15,000 employees. There were no documented exclusions to the participants or surveys. The study limitations consist of being a one-time cross-functional self-reported study, potential response bias and participants were provided different questions to cross-validate the hypothesis.
The study consisted of several demographic questions followed by violence prevention safety, management safety, work exhaustion and workplace violence exposure questions. The MSC questions differed between the two sample surveys and focused on management support and workplace safety promotion. The VPC questions were similar and included: "management in this organization quickly responds to episodes of violence," "management encourages employees to report physical violence," and "reports of violence from other employees are taken seriously by management.” The study participants were predominantly women (82%), typically white (60%) and African American (30%), had healthcare work experience ranging from 0-5 years (32%) to greater than 15 years (41%) and tenure in the organization was lower, with the majority (42%) having 0-5 years, 91% non-supervisors and 60% registered nurses.
The study supported the first two hypotheses and found that MSC positively correlates with VPC. Hamblin's research also found a negative correlation between VPC to quality of patient care, physical/psychological strain, workload and employee turnover rates. Hamblin suggests additional investigation should be done between MSC and VPC, as there are limited studies on MSC related to WPV.
Results
There are differences in healthcare employees' perspectives and their managers related to policies, training, and staffing.
Policies
The Christie study found that hospitals implemented zero-tolerance policies; however, employees believed managers do not comply with the policy as they fail to conduct adequate investigations, as well as a lack of employee victim support and lack of providing a safe environment. The study revealed that a low violence prevention culture resulted in employees failing to comply with the policy themselves.
Training
The Blando et al. study reflected a difference in perspectives between employees and managers. The study showed managers provided violence prevention training to employees to identify potentially aggressive individuals, warning signs and mitigation efforts. Blando et al. found that the behavioral health participants who had more WPV exposure and more training felt safer and had lower violence incidents.
However, Christie's study participants said the training was ineffective and better suited for security. These participants' perspectives lean toward violence occurring rather than identifying and preventing the escalation of violent behavior. The study also found that the participants wanted additional security personnel nearby as the nurses would not have severe injuries due to security's response and management.
Staffing
Blando et al. also found management invested in security and law enforcement resources to provide a safe environment. The study results found that injuries did not decrease with the additional resources, as the violence still occurred. However, employee satisfaction increased if security responded quickly and effectively, limiting the severity of the injury.
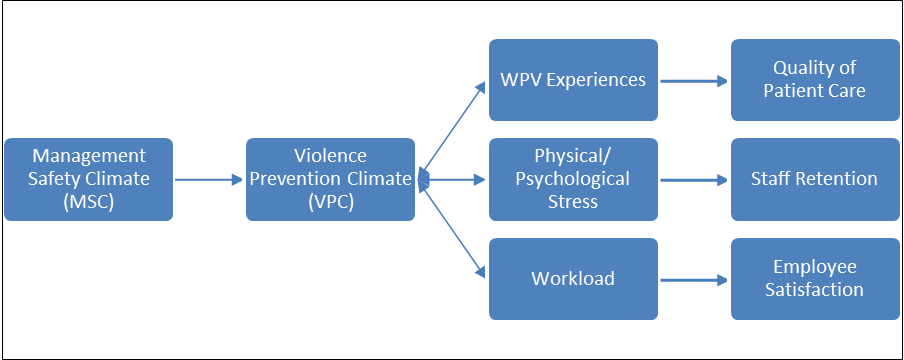 Figure 1: Correlation between MSC, VPC, Experiences, Stress and Workload
Figure 1: Correlation between MSC, VPC, Experiences, Stress and Workload
Kessler et al.'s study found that a low VPC negatively affects employee psychological strain, workload, quality of patient care and employee satisfaction. The Hamblin study also concluded that low VPC negatively affects employee satisfaction and retention rates. A positive violence prevention culture results in higher employee satisfaction, retention rates, and quality patient care (see Figure 1). Quality patient care affects patient satisfaction and patient volume. As such, business and financial resiliency depend on hospital managers fostering a positive violence prevention culture.
Employee Perspectives Impact WPV Program
Employee perspectives affect workplace violence programs as they may act differently. Employees can determine whether they adhere to the zero-tolerance policy, utilize skillsets to identify and reduce escalating behaviors and effectively use the workforce. A positive violence prevention culture results in higher employee satisfaction, retention rates and quality patient care.
Policies
The Kessler et al. and Hamblin studies confirm the Spector et al. VPC tool that measures employee perspectives on the violent climate and measures compliance with OSHA WPV guidelines. Spector found the VPC tool also identifies gaps in the WPV program, specifically in policy effectiveness, training, work safety climate and physical and psychological strain. Furthermore, Hamblin’s study confirmed that VPC strongly correlates with MSC. With the use of the VPC tool, managers can determine the compliance of the WPV program, safety culture and zero-tolerance policy, but they also may learn what is required to adjust their MSC as required.
Limitations
This article is limited to reviewing hyper-focused research conducted in U.S. hospitals within the past two decades related to employee perspectives, workplace violence and violence prevention climate. Most of the studies were cross-sectional studies, which could have had additional unknown research bias. Future research should conduct an experimental study investigating the relationship between MSC and VPC. Sample participants should include various hospitals of different sizes, states and units differentiating between the different unit types. Research should involve utilizing the MSC and VSC tools to compare previous study results. After identifying similar facilities, experiments should test changes to the elements to explore the relationship further.
Overall, a positive violence prevention culture results in higher employee satisfaction, retention rates and quality patient care. Future research should investigate the relationship between MSC and VSC testing changes to explore the relationship further.
This article originally ran in Security, a twice-monthly security-focused eNewsletter for security end users, brought to you by Security magazine. Subscribe here.
Looking for a reprint of this article?
From high-res PDFs to custom plaques, order your copy today!